What is seasonal affective disorder? Seasonal affective disorder (SAD) is a type of depression that follows a predictable seasonal pattern, most commonly beginning in late fall and continuing through winter before lifting in spring. It’s caused by reduced exposure to sunlight, which disrupts your circadian rhythm and affects levels of serotonin and melatonin in your brain. SAD is more than just “winter blues.” It’s a recognized clinical condition that can significantly impair daily functioning but responds well to treatment.
About 5 percent of American adults experience SAD, with symptoms lasting roughly 40 percent of the year. Women are four times more likely to be diagnosed than men, and the condition is more common at higher latitudes where winter days are shorter. If you find yourself struggling with the same depressive symptoms every winter and feeling fine by summer, you may be dealing with SAD rather than general depression.
What Causes Seasonal Affective Disorder
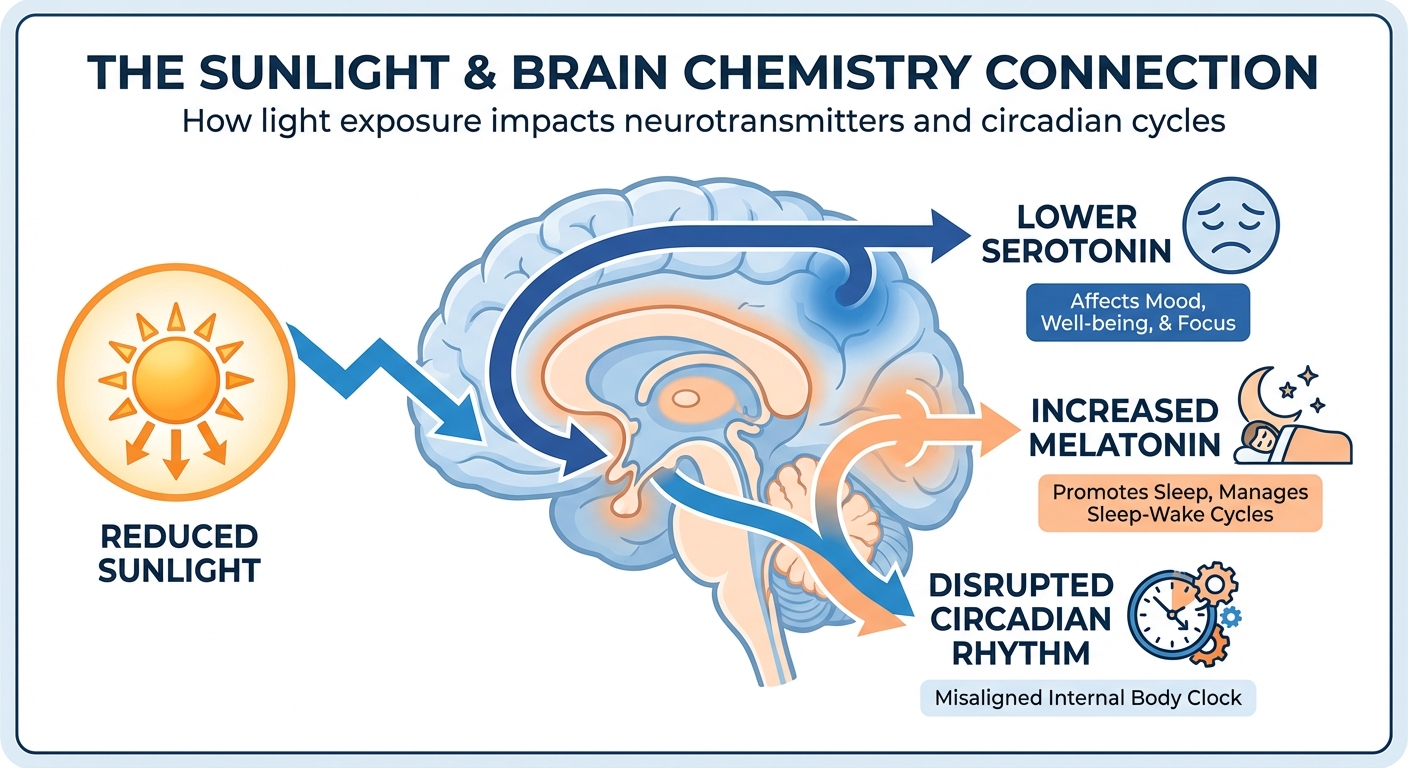
The primary trigger for SAD is reduced exposure to natural sunlight during shorter winter days. This light reduction affects your body in several interconnected ways, disrupting the biological processes that regulate mood, sleep, and energy.
Your circadian rhythm, the internal clock governing sleep-wake cycles and hormone release, depends on light exposure to stay calibrated. When you’re exposed to less daylight, your body’s clock can drift out of sync, making you feel tired at wrong times and disrupting sleep quality. This misalignment alone can cause mood symptoms, but it’s compounded by chemical changes.
Serotonin, a neurotransmitter that regulates mood, drops in response to decreased sunlight. Lower serotonin levels are strongly associated with depression. Simultaneously, your body produces more melatonin, the hormone that promotes sleep, in response to darkness. With longer nights and overcast days, melatonin production can increase, leaving you feeling drowsy and lethargic during waking hours. The combination of disrupted circadian rhythm, decreased serotonin, and increased melatonin creates the perfect conditions for seasonal depression.
Symptoms of Seasonal Affective Disorder
SAD shares many symptoms with major depression, but its seasonal pattern distinguishes it. Symptoms typically begin in October or November and resolve by March or April, though the timing varies by location and individual.
The most common symptoms include persistent low mood, loss of interest in activities you normally enjoy, difficulty concentrating, and changes in sleep patterns. Most people with winter SAD experience hypersomnia, sleeping more than usual yet still feeling tired. This contrasts with typical depression, which often causes insomnia. You may also experience increased appetite, particularly craving carbohydrates and comfort foods, often leading to weight gain.
Energy levels typically plummet. You might feel sluggish throughout the day regardless of how much you slept. Social withdrawal is common, with people turning down invitations and isolating themselves. This isolation can worsen symptoms, creating a negative feedback loop. Some people experience irritability, difficulty completing tasks, and physical symptoms like heaviness in the arms and legs.
The key diagnostic feature is the seasonal pattern. If you experience these symptoms every winter for at least two consecutive years, with full remission in spring and summer, and if seasonal episodes substantially outnumber non-seasonal episodes in your history, SAD is the likely diagnosis. However, only a healthcare provider can make an official diagnosis and rule out other conditions.
Treatment Options for SAD
SAD responds well to several treatment approaches, often used in combination. The most distinctive treatment is light therapy, which directly addresses the reduced light exposure that triggers symptoms.
Light therapy involves sitting near a special light box that emits bright light mimicking natural outdoor light. The standard recommendation is 10,000 lux for 20 to 30 minutes each morning, positioned at eye level but not stared at directly. Most people notice improvement within a few days to two weeks. Light therapy is most effective when used consistently throughout the winter months, starting in early fall before symptoms begin.
Antidepressant medications, particularly SSRIs like sertraline and fluoxetine, can effectively treat SAD. Some people take medication only during winter months, starting in fall and tapering off in spring. Bupropion extended-release is specifically FDA-approved for preventing seasonal depression and is often started before symptoms appear.
Cognitive behavioral therapy adapted for SAD, called CBT-SAD, helps people identify and change negative thought patterns associated with winter and darkness. It also incorporates behavioral activation, scheduling pleasant activities to counteract the tendency toward withdrawal. Studies show CBT-SAD may have longer-lasting effects than light therapy, with lower recurrence rates in subsequent winters.

Lifestyle Changes That Help
Beyond formal treatments, certain lifestyle modifications can reduce SAD symptoms and work synergistically with medical approaches.
Maximizing natural light exposure is fundamental. Open blinds and curtains first thing in the morning. Sit near windows when possible. Take walks outside during daylight hours, even when overcast, since outdoor light is typically brighter than indoor lighting even on cloudy days. Exercise outdoors when weather permits to combine light exposure with physical activity.
Regular exercise has proven antidepressant effects. Aim for 30 minutes of moderate activity most days. The type matters less than consistency, though outdoor exercise provides additional light exposure benefits. Exercise releases endorphins, reduces stress hormones, and can improve sleep quality, addressing multiple SAD symptoms simultaneously.
Maintain a consistent sleep schedule even when you feel like sleeping longer. Going to bed and waking at the same times helps regulate your circadian rhythm. Avoid oversleeping on weekends, which can worsen circadian disruption. If you’re using light therapy, do it immediately upon waking to anchor your morning routine.
Social connection counteracts the isolation tendency. Make advance plans with friends or family, making it harder to cancel when you’re feeling low. Let close friends know you struggle in winter so they can check in and offer support. Consider joining a winter activity group to create built-in social obligations.
When to Seek Professional Help
While mild winter blues may respond to self-care, clinical SAD requires professional treatment. Seek help if symptoms interfere with work, relationships, or daily functioning. If you’re sleeping through alarms, missing work, or struggling to complete basic tasks, it’s time to see a healthcare provider.
Warning signs that require immediate attention include thoughts of suicide or self-harm, significant increase in alcohol or substance use to cope, complete inability to function, or symptoms that persist into spring and summer. These may indicate more serious depression requiring urgent intervention.
Start with your primary care provider, who can evaluate symptoms, rule out other conditions like hypothyroidism that can mimic SAD, and provide or refer for treatment. A mental health professional can offer therapy options. Many people benefit from seeing both a prescriber for medication and a therapist for CBT-SAD.
Don’t wait until symptoms become severe. If you know you struggle every winter, see your provider in early fall to establish a prevention plan. Starting light therapy or medication before symptoms emerge is often more effective than treating established depression.
Summary
Seasonal affective disorder is a form of depression triggered by reduced winter sunlight, which disrupts circadian rhythms and brain chemistry affecting mood and energy. Symptoms include persistent sadness, fatigue, oversleeping, carbohydrate cravings, and social withdrawal, following a predictable pattern of onset in fall and remission in spring.
Effective treatments include light therapy, antidepressant medication, and cognitive behavioral therapy tailored for SAD. Lifestyle changes like maximizing light exposure, exercising regularly, and maintaining social connections provide additional benefit. If symptoms interfere with daily life, seek professional help, ideally before winter begins, to prevent or minimize impact.